
Late on November 10, 2025, 54-year-old Mr. Liu was urgently admitted to the DSA operating room due to persistent hemoptysis.Under the precise management of the medical team led by Director Huang Deliang, the procedure concluded successfully within an hour, effectively controlling the bleeding.
As he emerged from anesthesia, Mr. Liu's breathing steadied and his consciousness cleared—a moment mirroring another critical night in February 2022, when he underwent emergency surgery for severe respiratory distress, also performed by Director Huang. These two midnight surgeries, both turning crisis into safety, stand as testament to five years of trust and perseverance between doctor and patient.
The Long Road to Treatment: A Story Beginning with Hemoptysis
In March 2020, Mr. Liu received emergency interventional embolization at a local people's hospital for sudden hemoptysis. A postoperative biopsy confirmed poorly differentiated squamous cell lung carcinoma, marking the start of a five-year battle against cancer. His thick medical record documents every step—from particle implantation and tracheal stenting to local ablation and arterial perfusion chemotherapy. Throughout this journey, he consistently returned to the medical team led by Director Huang at each critical juncture.
The morning after his latest surgery, Director Huang arrived for rounds as usual. Mr. Liu, now able to sit by the bed and speak clearly, listened as his wife softly remarked, "Over these five years, Director Huang has saved him time and again..." Her voice trembled before she could finish, and she bowed deeply to Director Huang—a gesture carrying five years of unspoken trust and gratitude from an entire family.
The First Life-or-Death Battle: The Fight for Breath in February 2022
That winter, Mr. Liu was rushed to a hospital in Guangzhou with severe breathing difficulties. A bronchoscopy revealed complete blockage of both main bronchi by tumor tissue, nearly closing off his airway and placing his life in imminent danger. Director Huang, then away from the city, assessed the situation and rushed back overnight, heading straight to the operating room to lead the rescue effort.
Guided by bronchoscopy, Director Huang's team began a meticulous and prolonged tumor ablation surgery. The extensive and complex nature of the lesions meant the surgery lasted nearly five hours.

Using microwave ablation, the team carefully removed the obstructive tumor tissue, gradually reopening the airway. When the final blockage was cleared and ventilation was restored to both lungs, the oxygen saturation on the monitor steadily climbed—the pathway to life had finally been reopened.
This was not only a technical challenge but also a test of physical and mental endurance. The five-hour, non-stop surgery not only relieved the patient's critical condition but also bought precious time for subsequent treatments.
Analysis of Microwave Ablation Technology
A thin ablation needle is inserted into the tumor site. Under a high-frequency microwave electric field, water molecules within the tumor tissue rapidly rotate and generate friction, producing localized temperatures of 60–100°C. This causes coagulative necrosis of the tumor cells, effectively "burning" the tumor away.
The Second Life-or-Death Battle: The Fight Against Hemoptysis in November 2025
In September of this year, Mr. Liu's main tracheal stent was removed after displacement, and his condition stabilized temporarily. However, intermittent hemoptysis beginning in early November brought him back to critical condition. Imaging revealed active bleeding in the intercostal-bronchial common trunk artery and the right internal thoracic artery.
The surgery, which began at 11 PM on November 10, involved Director Huang's team performing the following steps in sequence:
1)Angiography of the intercostal-bronchial common trunk artery
2)Superselective angiography, perfusion, and embolization of the right bronchial artery
3)Superselective angiography, perfusion, and embolization of bilateral bronchial arteries
4)Superselective angiography, perfusion, and embolization of the right internal thoracic artery
The procedure concluded in the early hours of the following morning. Mr. Liu's hemoptysis was effectively controlled, and his oxygen saturation returned to safe levels. In that moment, everyone in the operating room breathed a sigh of relief—once again, a life had been pulled back from the brink.
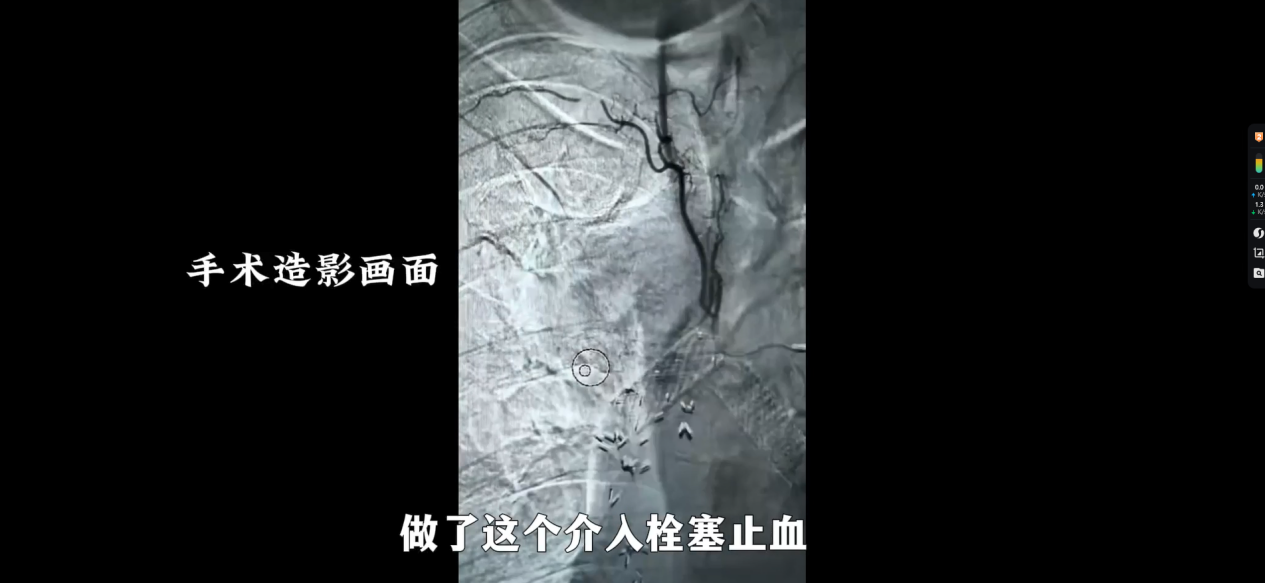
Explanation of Superselective Angiography, Perfusion, and Embolization
Under DSA guidance, a microcatheter is superselectively inserted into the tumor's feeding arteries. Contrast agent is first injected to clearly visualize the tumor's vascular distribution. High-concentration chemotherapeutic drugs are then perfused directly into the lesion, followed by embolization particles to block the tumor's blood supply—achieving the dual goals of "precision drug delivery" and "cutting off its supply lines."
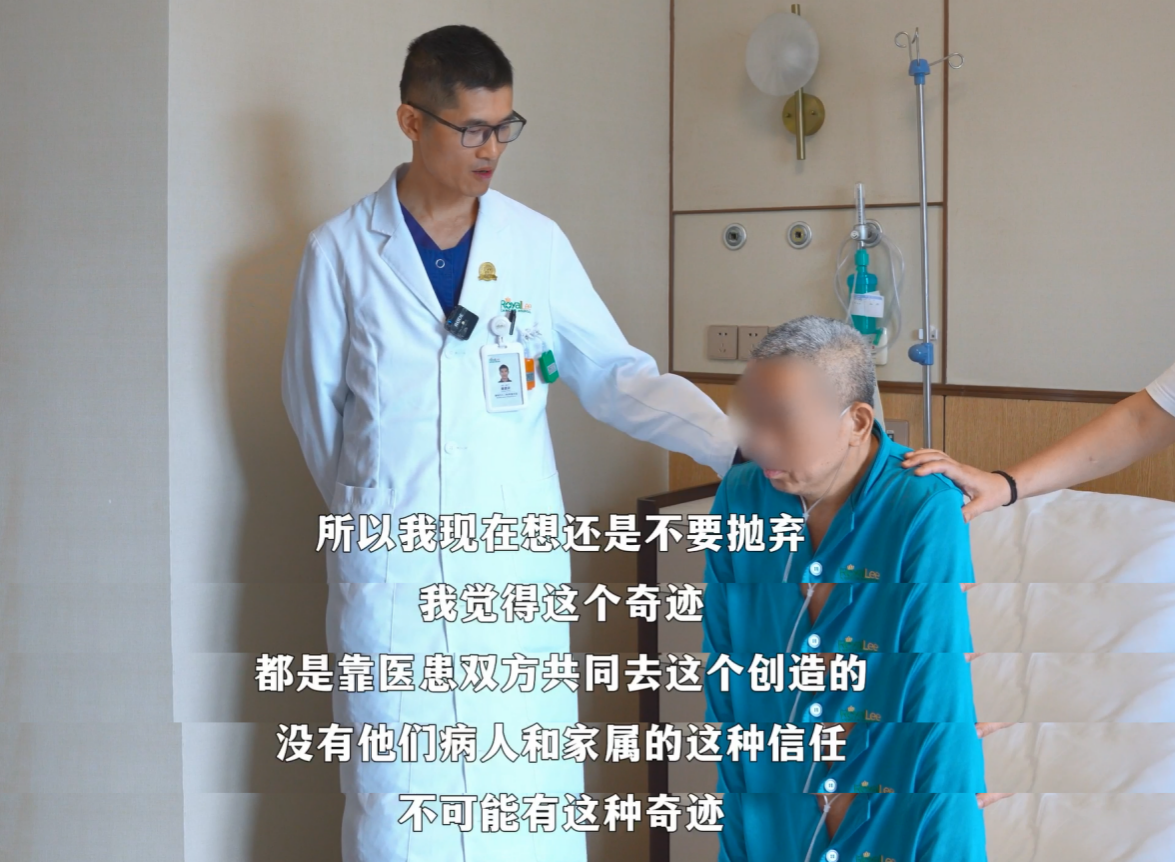
Five years fighting cancer, two life-or-death crises. Mr. Liu's experience not only highlights the critical role of modern interventional medicine in treating severe, acute conditions but also reaffirms the invaluable power of trust and persistence in the doctor-patient relationship.


 (+86)18613012387
(+86)18613012387 info@royallee.cn
info@royallee.cn EN
EN CN
CN TH
TH IDN
IDN  AR
AR




