So how should pancreatic cancer be dealt with? With the advancement of technology, the "savior" for pancreatic cancer has emerged—the NanoKnife ablation technique!
In early December, in the DSA operating room of Guangzhou Royal Lee Cancer Center, Dr. Huang Deliang, the Director of Minimally Invasive Treatment Center, assisted by the hospital's Imaging Department and Anesthesiology Department, performed NanoKnife ablation surgery on a 71-year-old pancreatic cancer patient.

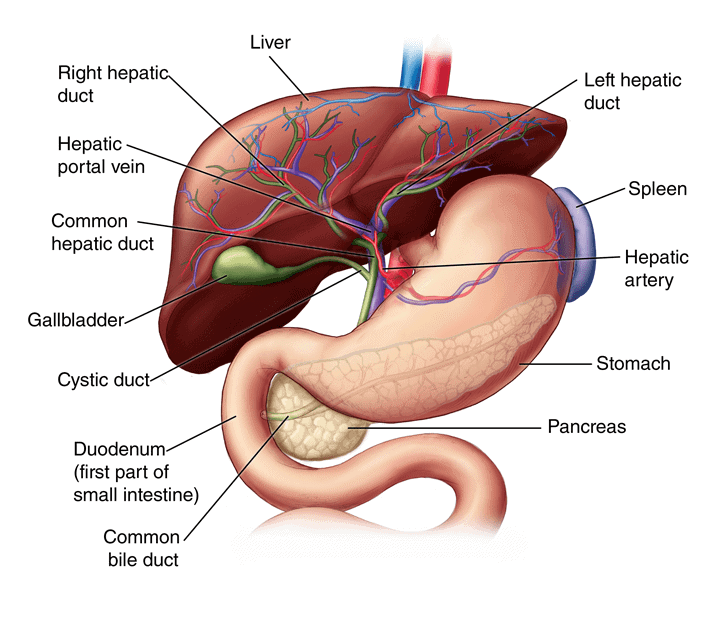
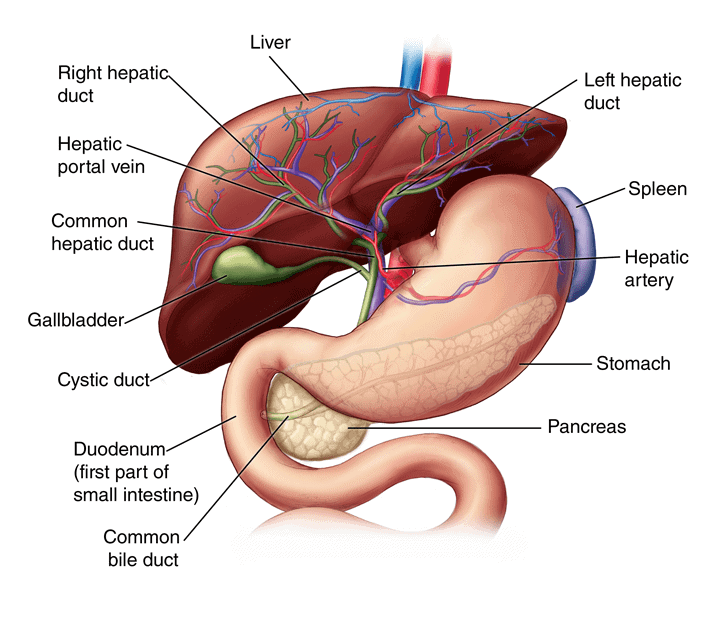
The pancreas is an elongated gland, situated horizontally at the level of the 1st to 2nd lumbar vertebrae on the posterior abdominal wall. Its location is relatively concealed and in close proximity to several vital organs, posing potential risks. With a unique tissue structure, it features abundant glandular elements. Therefore, during NanoKnife treatment, precise needle placement (electrode needle) is crucial, demanding a high level of technical skill from the medical practitioner.
And this surgery at Royal Lee is even more special—because four needles need to be placed. "Among all the NanoKnife surgeries coordinated with many hospitals by our research and development manufacturer, performing surgery with the placement of four needles and completing it smoothly within 2 hours is considered a highly challenging procedure!" stated the person in charge at Alpmed.
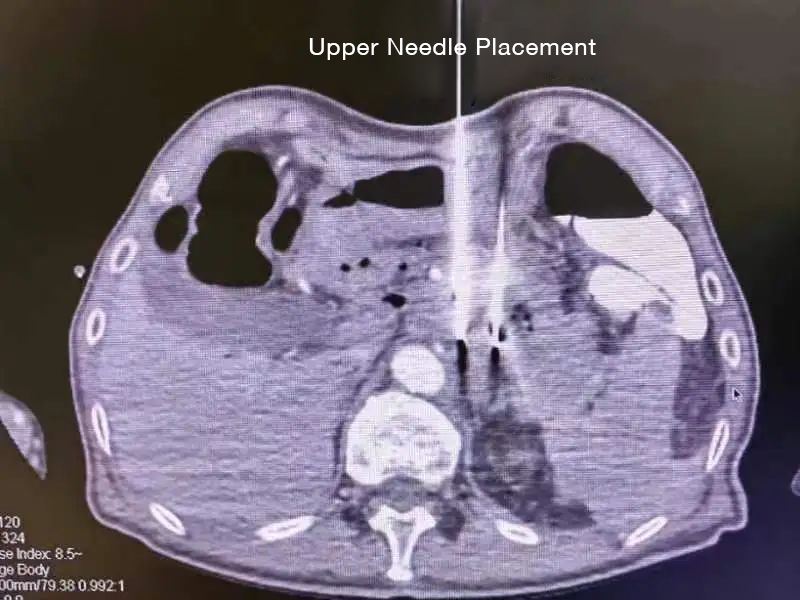
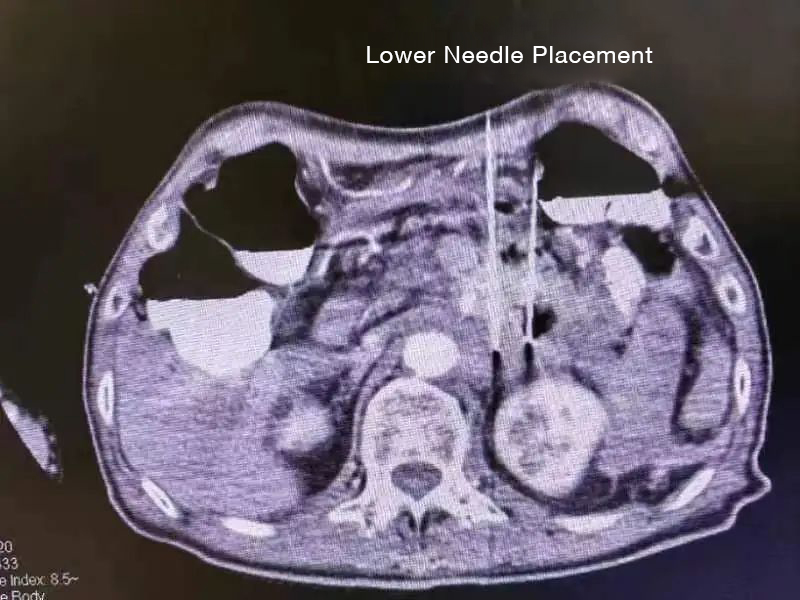
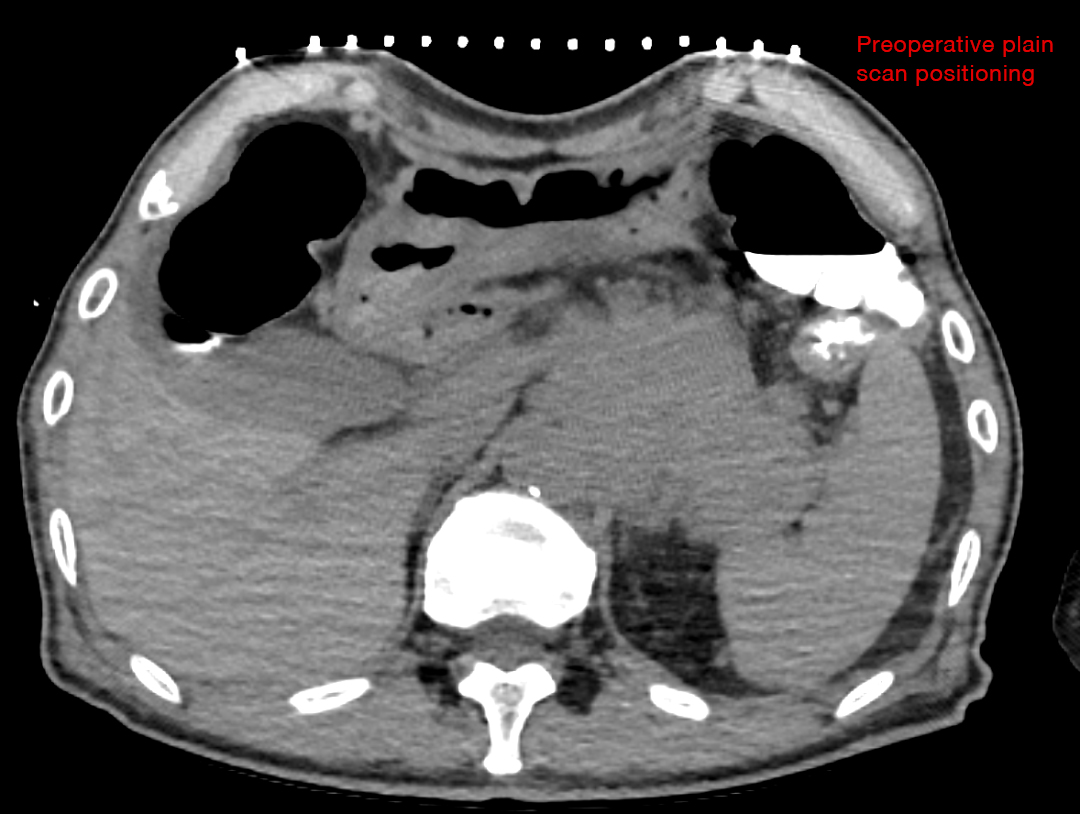
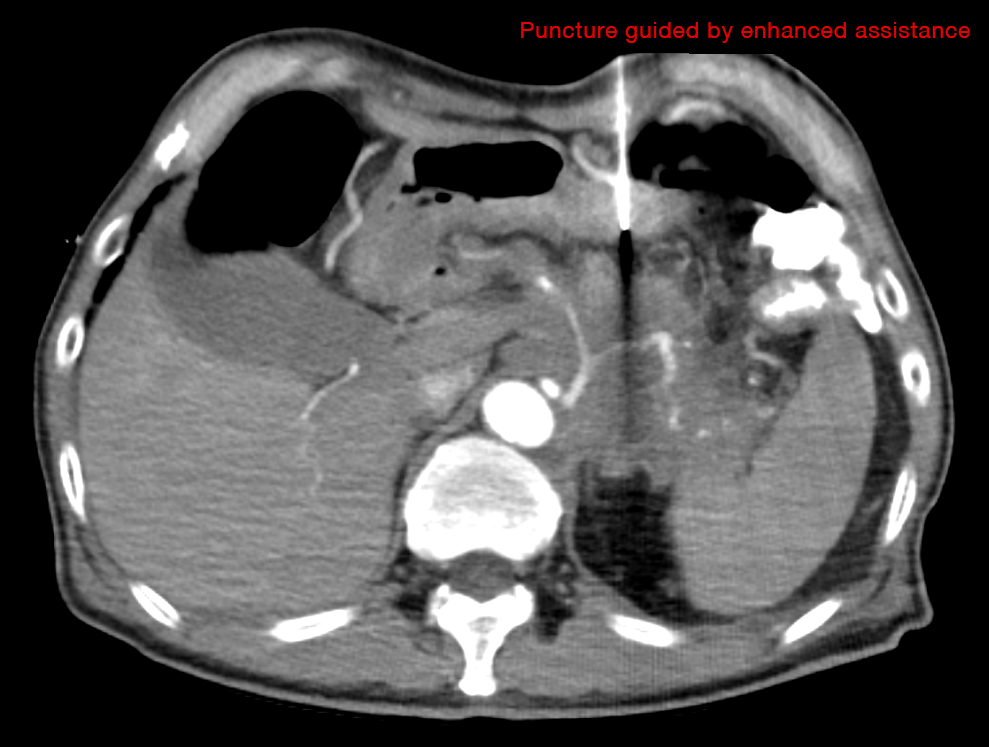
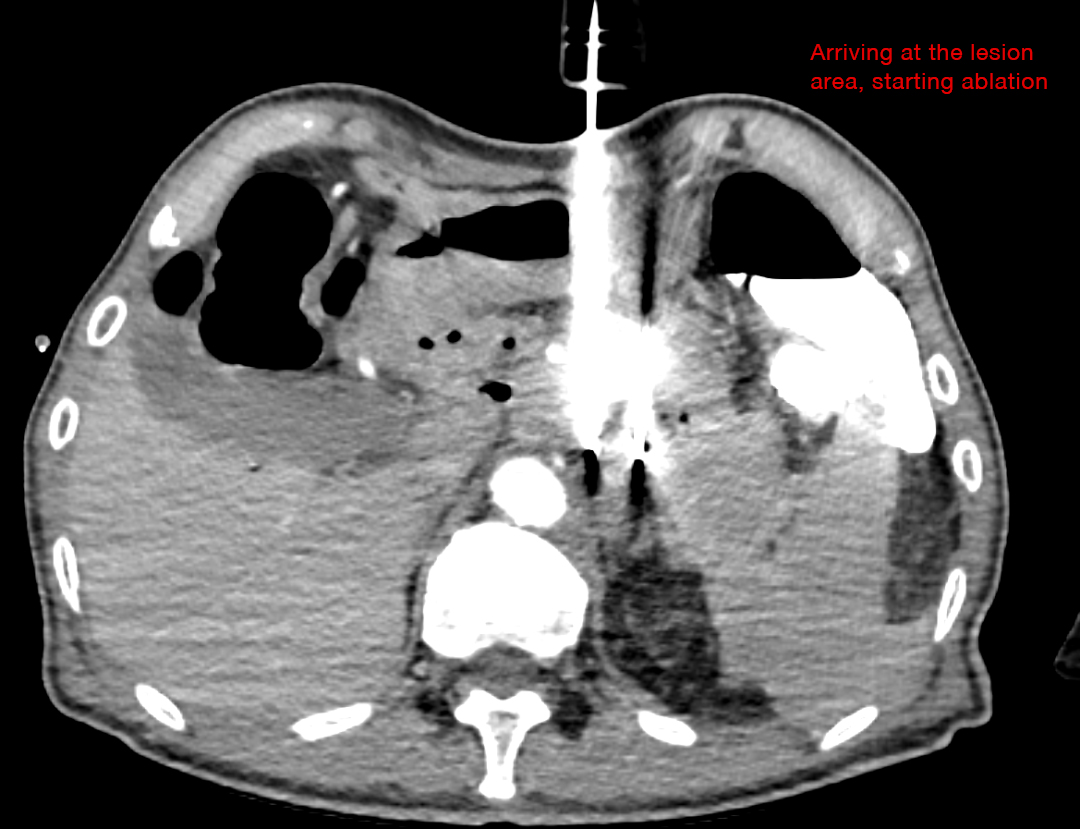
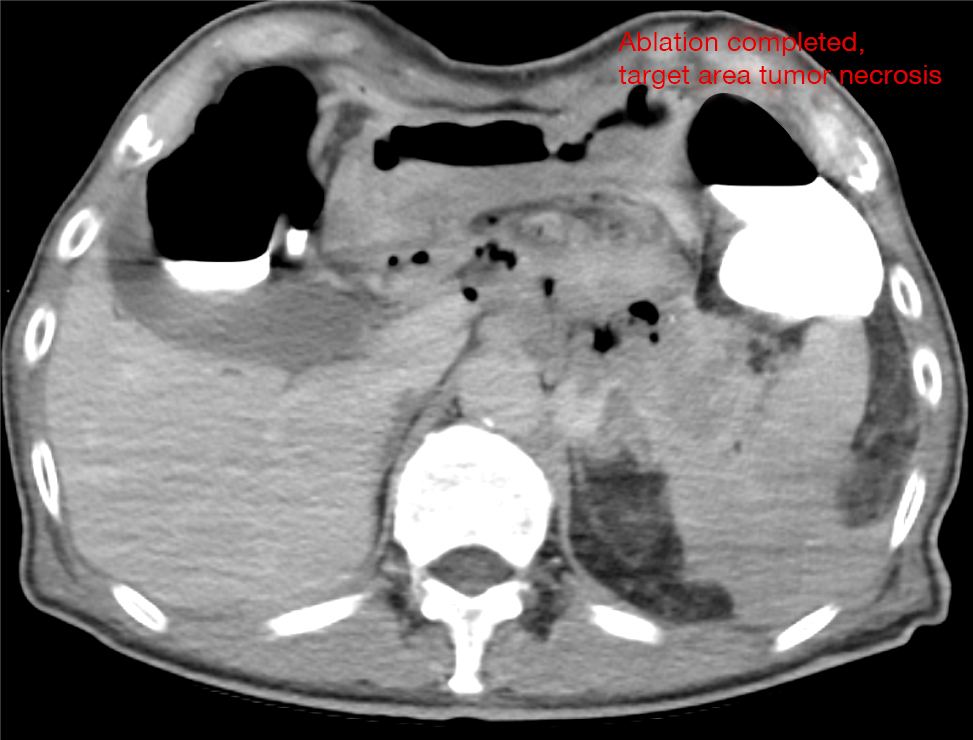
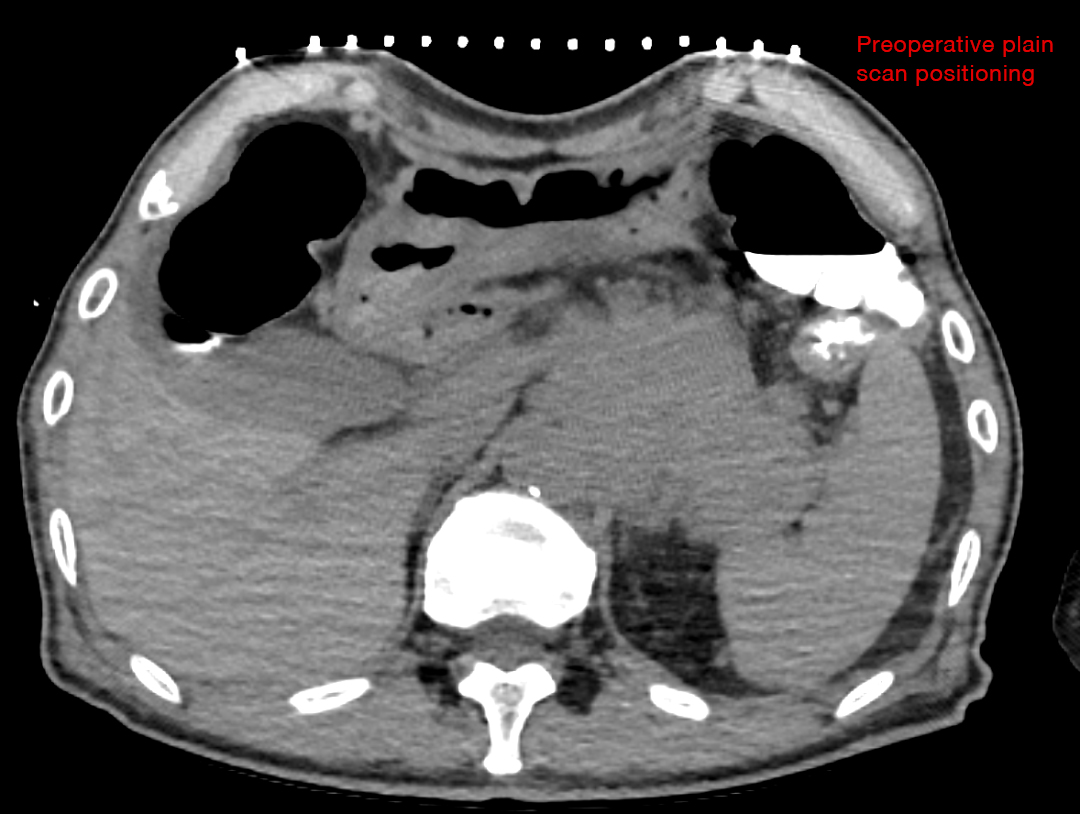
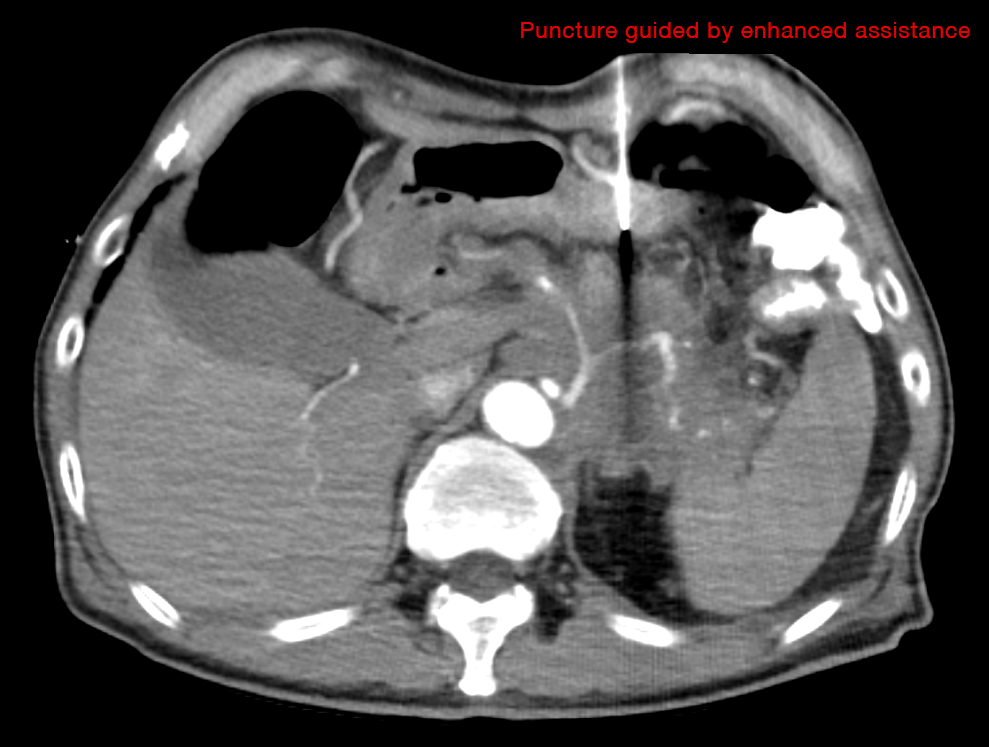
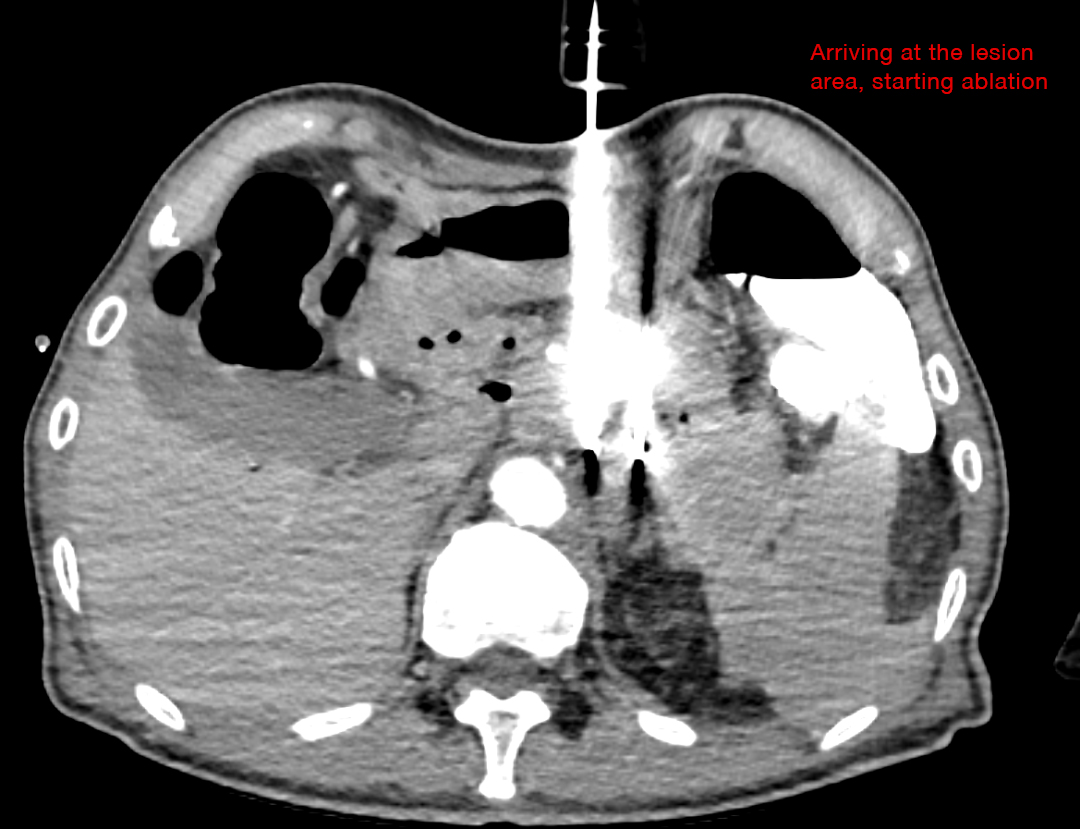
Dr. Huang Deliang is completely focused during the surgery. Under ultrasound guidance, the distance between each needle is only 2cm. Dr. Huang must navigate around vital tissues such as blood vessels and nerves. However, he skillfully maneuvers, avoiding blood vessels with precision, perfectly safeguarding them, and ensuring accurate needle placement. As seen in the postoperative CT, the surrounding blood vessels are clearly visible in the contrast imaging. No signs of leakage or bleeding are observed in the abdominal cavity. Significant changes are evident before and after the surgery, with pronounced gasification in the tumor area and no enhancement on contrast—simply put, it means that no obvious malignant lesions were found postoperatively!
So, how does NanoKnife ablation work to eliminate cancer cells? The editor obtained authoritative information from Director Huang Deliang, as well as the NanoKnife development company. The following information will provide some insights.

Director Dr. Huang Deliang (left) performing NanoKnife surgery on the patient.
The pancreas is an elongated gland, situated horizontally at the level of the 1st to 2nd lumbar vertebrae on the posterior abdominal wall. Its location is relatively concealed and in close proximity to several vital organs, posing potential risks. With a unique tissue structure, it features abundant glandular elements. Therefore, during NanoKnife treatment, precise needle placement (electrode needle) is crucial, demanding a high level of technical skill from the medical practitioner.
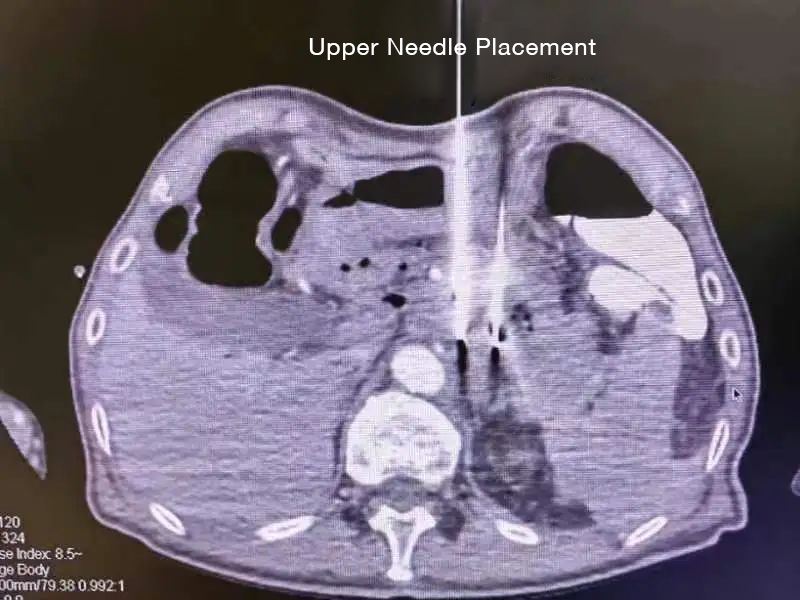
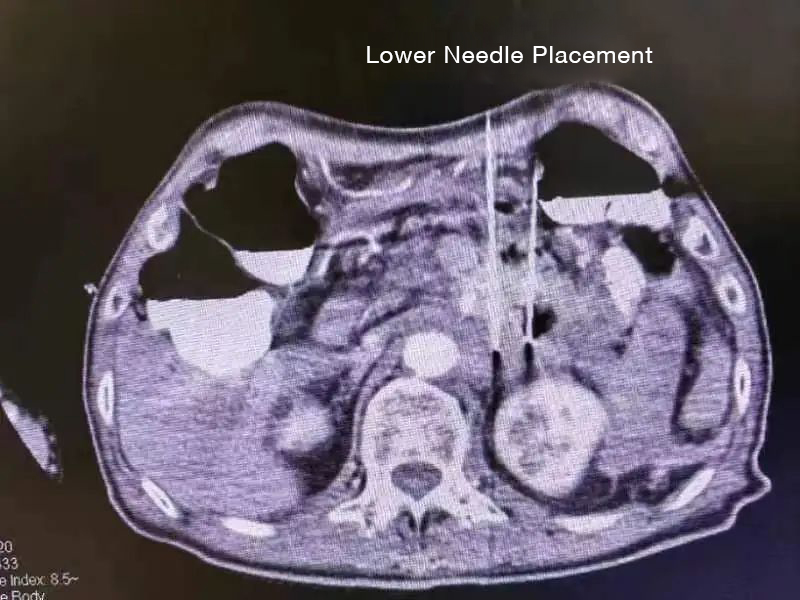
Needle Placement
And this surgery at Royal Lee is even more special—because four needles need to be placed. "Among all the NanoKnife surgeries coordinated with many hospitals by our research and development manufacturer, performing surgery with the placement of four needles and completing it smoothly within 2 hours is considered a highly challenging procedure!" stated the person in charge at Alpmed.
Dr. Huang Deliang is completely focused during the surgery. Under ultrasound guidance, the distance between each needle is only 2cm. Dr. Huang must navigate around vital tissues such as blood vessels and nerves. However, he skillfully maneuvers, avoiding blood vessels with precision, perfectly safeguarding them, and ensuring accurate needle placement. As seen in the postoperative CT, the surrounding blood vessels are clearly visible in the contrast imaging. No signs of leakage or bleeding are observed in the abdominal cavity. Significant changes are evident before and after the surgery, with pronounced gasification in the tumor area and no enhancement on contrast—simply put, it means that no obvious malignant lesions were found postoperatively!
So, how does NanoKnife ablation work to eliminate cancer cells? The editor obtained authoritative information from Director Huang Deliang, as well as the NanoKnife development company. The following information will provide some insights.
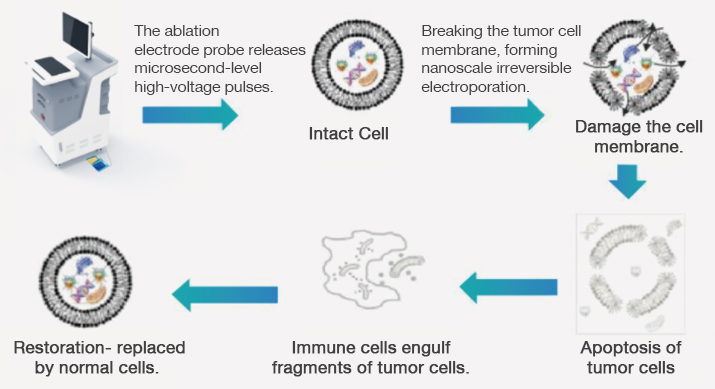
NanoKnife, also known as Irreversible Electroporation (IRE) ablation technology, is an emerging tumor ablation technique that does not rely on thermal energy. It utilizes minimally invasive electrodes to deliver microsecond-level electrical pulses, forming an electric field surrounding the tumor. The electric field energy acts on the phospholipid bilayer of the cell membrane, creating multiple nanoscale pores on the cell surface. This leads to an increase in cell membrane osmotic pressure, causing the outflow of cellular fluid. When the pulse energy exceeds a certain electric field threshold, irreversible cell damage occurs, triggering cell apoptosis. Importantly, it has the characteristic of protecting vital structures such as nerves, glands, pancreatic ducts, large blood vessels, and bile ducts.
Therefore, IRE technology is a crucial option for treating unresectable pancreatic cancer that is adjacent to or surrounds important lumens such as the abdominal cavity, portal vein, and bile duct. Numerous clinical research results indicate that NanoKnife treatment for pancreatic cancer has an excellent prognosis, significantly extending the patient's survival period and providing a new lease of life for patients!
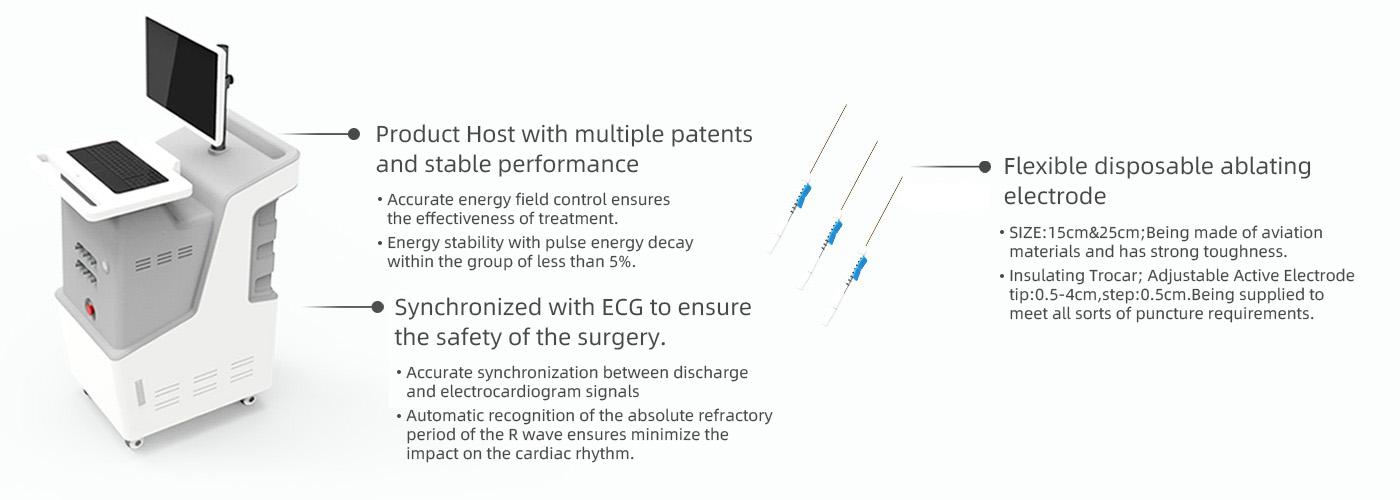
The principles of NanoKnife tumor ablation:
Step 1: The ablation electrode probe releases microsecond-level high-voltage pulses.
Step 2: Breaking the tumor cell membrane, forming nanoscale irreversible electroporation.
Step 3: Collapse of the tumor cell structure.
Step 4: Apoptosis of tumor cells.
Step 5: Immune cells engulf fragments of tumor cells.
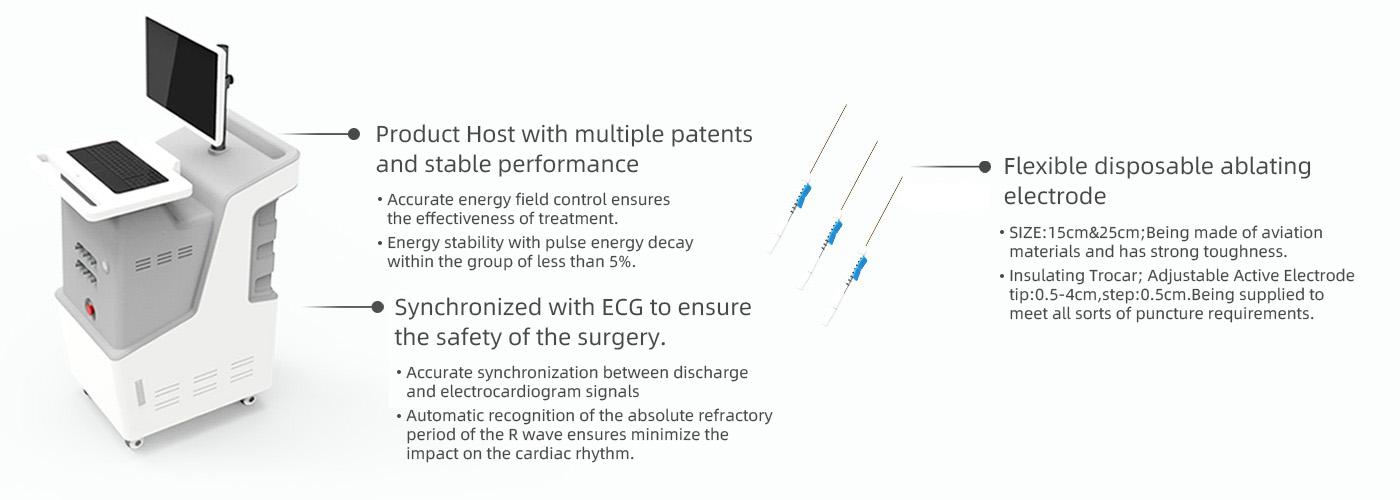
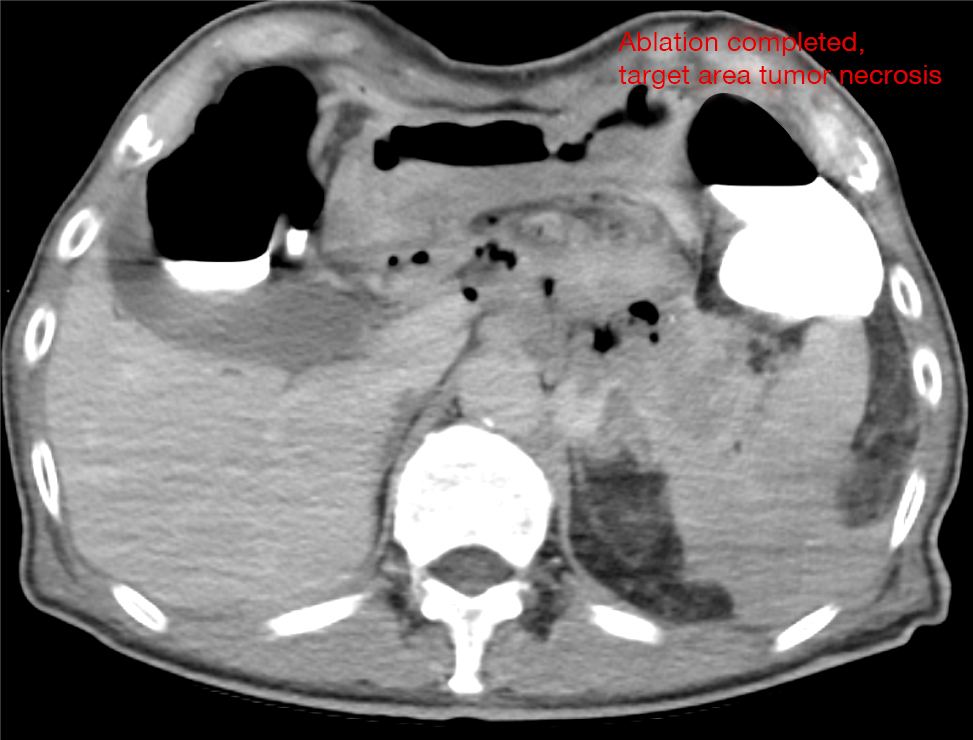
IRE High Voltage Steep Pulse Therapeutic System
The principles of NanoKnife tumor ablation:
Step 1: The ablation electrode probe releases microsecond-level high-voltage pulses.
Step 2: Breaking the tumor cell membrane, forming nanoscale irreversible electroporation.
Step 3: Collapse of the tumor cell structure.
Step 4: Apoptosis of tumor cells.
Step 5: Immune cells engulf fragments of tumor cells.
The advantages of NanoKnife technology:
1. Compared to other ablation therapies, the energy is more concentrated, and the duration is shorter.
2. Blood vessels, nerves, and other structures in the treatment area are not damaged, ensuring good safety.
3. Thorough treatment with clear treatment boundaries.
4. Real-time monitoring of the treatment process ensures treatment integrity.
5. It can be operated under the guidance of ultrasound (B-mode) and CT, and can also be used for ablative treatment of isolated metastases discovered during surgical procedures.
6. Strong operability and compatibility in terms of treatment approach, access, and physician operation.
7. The treated area can be rapidly replaced by normal cells, restoring normal function.
Which tumors are suitable for NanoKnife technology treatment?
It is suitable for liver, lung, kidney, pancreatic, and isolated solid metastatic tumors in the abdominal cavity, with tissue targeting.
It has unique advantages in treating cases near the porta hepatis, gallbladder, intestines, pancreatic tumors, or cases where surgery is not applicable or for postoperative recurrence.
Applicable Population:
- Cancer patients for whom conventional ablation methods are difficult to handle.
- Patients who are not suitable or unwilling to undergo surgery or chemotherapy.
- Cancer patients with postoperative recurrence who cannot tolerate surgery again.
- Cancer patients with poor outcomes after traditional surgery, radiotherapy, or chemotherapy.
- Individuals who develop tolerance and adverse reactions to radiotherapy and chemotherapy.
Contraindications:
- Presence of implanted cardiac pacemakers or defibrillators in the ablation area.
- Implantation of electronic devices and metal parts within a 2cm range of the ablation area.
- Ablation in the eye area, including the eyes and face.
- Patients with a history of epilepsy or severe arrhythmias.
- Patients who have recently experienced a myocardial infarction.


 (+86)18613012387
(+86)18613012387 info@royallee.cn
info@royallee.cn EN
EN CN
CN TH
TH IDN
IDN  AR
AR